Rebecca Mount, DVM, DACVD
1. Clinical signs of bacterial pyodermas
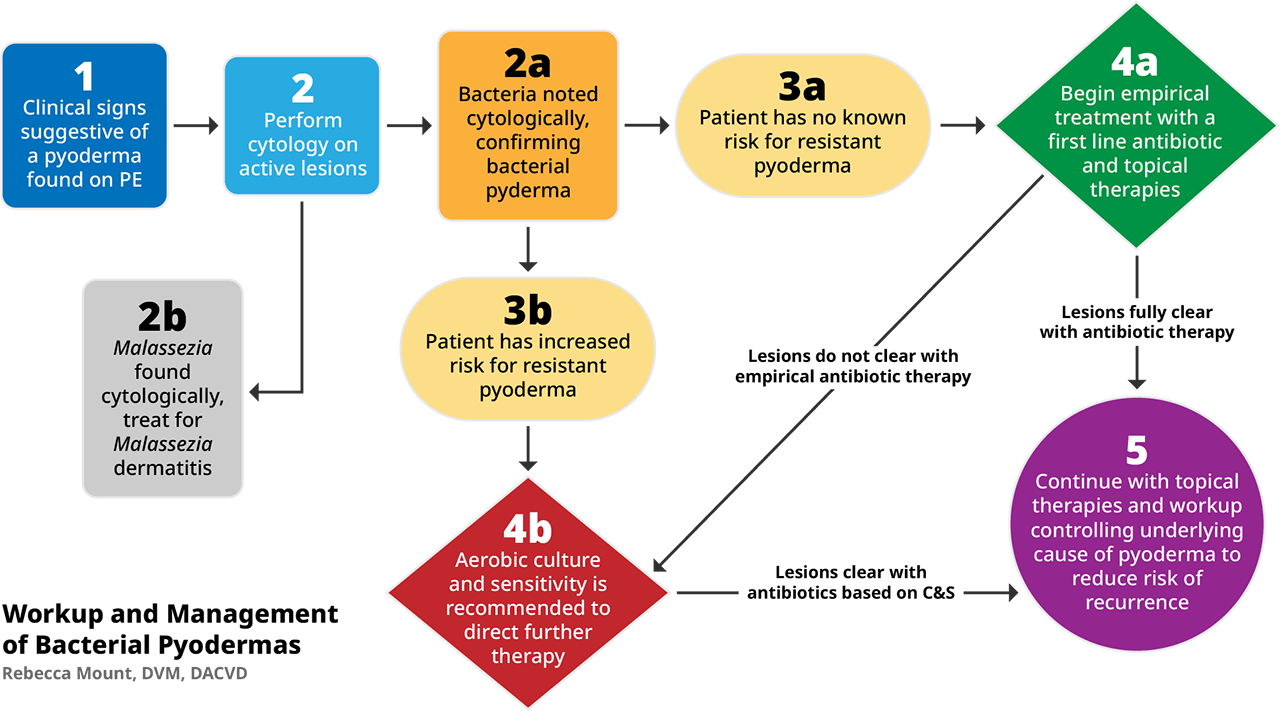
Bacterial skin infections (aka pyodermas) are a very common reason that pets present to their veterinarians for care. Additionally, pyodermas are one of the most common reasons for antibiotic use in small animal practice5. With the emerging increase in the number of resistant infections seen in practice, it is imperative to understand the work up for management of this common skin ailment.
The most common cutaneous pathogen associated with pyodermas in veterinary medicine is Staphylococcus pseudintermedius. Other staphylococcal species1, including S. schleiferi, other coagulase negative staphylococcal species, and S. aureus have also been associated with pyodermas. Less common cutaneous pathogens include: Pseudomonas spp., Streptococcus spp., and Corynebacterium spp1,2.
Pyodermas are often classified by the depth of infection (superficial or deep), frequency of infection (initial infection or recurrent), and by distribution of lesions (localized or generalized).
- Superficial Pyodermas: Result in skin lesions which are confined to the epidermis and follicular epithelium. Lesions include2,5: erythema, papules, pustules, epidermal collarettes, and crusts.
- Deep Pyodermas: As the name implies the infection affects the deeper layers of the skin, including the dermis. Lesions include2,5: nodules, ulcerations, draining tracts with exudate, and bullae.
With both superficial and deep pyodermas odor and pruritus can be variable.
Judicious use of antibiotics is imperative to help reduce the risk of developing resistant bacterial pyodermas. Therefore, even with supportive clinical lesions, it is important to confirm the presence of bacteria with cytology and/or a culture before initiating treatment with antibiotics.
2. Cytological evaluation of skin lesions
Unfortunately, there is no easy way to determine the cause of skin lesions by look, touch, or smell alone. Cytology is a vital part of the dermatological work up and is the best way to ensure that treatment recommendations are valid.
Cytology is a relatively easy point of care test that evaluates for the presence of inflammatory cells, infectious agents including bacteria and Malassezia spp., and atypical cells suggestive of neoplastic factors. It is important to describe the quantity of bacteria (1-4+), the size and shape of the bacteria seen, and if the bacteria is found intracellularly or extracellularly.
There are many methods for collecting cytological samples including2,5:
- Adhesive tape strips
- Impression smears
- Swabs
- Fine needle aspirates
Additionally, cytology is an invaluable tool for measuring response to antimicrobial therapy. Quantification of bacteria prior to starting antibiotics allows for a semi-objective measurement of therapeutic results. If bacteria is still present on serial cytological samples during and post antibiotic therapy, a resistant pyoderma should be considered.
3a & 3b. Risk Factors for development of resistant pyoderma:
Before determining antibiotic selection, each patient’s history should be closely evaluated for potential risk factors for the development of resistant pyodermas. If a pet has one or more of the risk-factors1,4,5 below, a bacterial culture is recommended prior to initiating antibiotic therapy.
- Systemic antibiotic therapy, for any reason, within the last 6 months.
- Treatment with steroids within the previous 6 months.
- Veterinary contact, especially hospitalizations, within the last 4 weeks.
- Repeated history of antimicrobial therapy.
- Incomplete duration or dose of historical antibiotic therapy.
Previous use of fluoroquinolones as a first line antibiotic.
4. Empirical treatment vs. Culture and Sensitivity for treatment
4a: Empirical therapy is commonly used for non-complicated bacterial pyodermas in low-risk patients. When using empirical therapy, it is important to follow the antimicrobial stewardship guidelines including the use of appropriate antibiotic class, dosage, and duration of treatment. The most current antimicrobial guidelines1 for superficial bacterial infections recommend only using tier 1 antibiotics for empirical treatment of pyodermas.
Tier 1 antibiotics include:
- Clindamycin
- 1st generations cephalosporins (cephalexin, amoxicillin-clavulanate)
- Potentiated sulfonamides
- +/- 3rd generation cephalosporins (cefpodoxime, cefovecin)
A minimum antibiotic course of 3 weeks or 1-week past resolution of clinical signs2 is recommended for a superficial bacterial pyoderma, while a minimum of 4-6 weeks of antibacterial therapy is recommended for a deep pyoderma.
Topical therapies are beneficial in all pyoderma cases. Shampoos, mousses, sprays, and/or ointments may be recommended as sole therapies for localized lesions or in conjunction with systemic antibiotics for more widespread bacterial pyoderma. In mild cases of widespread pyodermas, a topical regimen may be sufficient for clearing the superficial bacterial skin infection.
4b: A bacterial culture is never contraindicated, however in certain cases culture is more imperative than others.
Reason to culture before starting antimicrobial therapy1:
- Lack of resolution of lesions and cytological evidence of bacteria despite appropriate course of an empirical antibiotic.
- Development of new lesions while on an empirical antibiotic course.
- History of multi-drug or methicillin resistant pyoderma
- Presence of rods on cytology
- The pet has one or more risk factor for development of resistant pyoderma
How to maximize your culture samples:
Best lesions for culturing a superficial pyoderma2:
- Intact pustules-Rupture with a sterile needle and collect the exudate on the culture swab
- Crusts- Gently lift an intact crust and swab the exudate beneath the crust
- Epidermal collarettes-Swab under the spreading edge of the collarette
- Rupturing a bulla or aspirating a nodule
Best Lesions for culturing a deep pyoderma:
- Deep tissue cultures are ideal for deeper infections-Avoids contamination from superficial microbes
- Exudate from draining tracts-May have contamination of superficial organisms
For most superficial and deep pyoderma an aerobic is recommended. Anaerobic cultures are only required if atypical bacteria is suspected.
Interpreting your culture results and selecting treatment:
In some cases, culture will detect both cutaneous pathogens and contaminants. It is important to look at the results in light of the clinical presentation and cytological findings1,2,5. It is important to focus on the most common cutaneous pathogens, such as staphylococcal species and Pseudomonas spp.
The use of tier 2 and 3 antibiotics1 should only be considered based on culture and sensitivity findings. Tier 3 should be used sparingly as they are generally reserved for treatment of serious methicillin resistant infections in humans.
Tier 2 antibiotics include:
- Doxycycline and Minocycline
- Chloramphenicol
- Fluroquinolones
- Aminoglycosides
- Rifampicin
Tier 3 antibiotics include:
- Linezolid
- Teicoplanin
- Vancomycin
The duration of therapy should be dictated based on the depth of the lesions similar to empirical therapy. Topical therapies are also extremely important for the short-term and long-term management of a resistant pyoderma and should be considered in all cases.
5. Working up the underlying cause and long-term use of topical therapies
Prevention of recurrent pyodermas is imperative to reduce the use of systemic antibiotics and subsequent risk of developing resistant pyodermas. Prevention is generally two-fold requiring both the diagnosis and management of the underlying cause and long-term maintenance therapy with topicals to reduce bacterial carriage and risk of reoccurrence.
The most common underlying diseases2 that predispose pets to develop bacterial skin infections are:
- Allergic Disease
- Flea bite hypersensitivity
- Parasite hypersensitivity (sarcoptic mange, demodectic mange, and cheyletiellosis)
- Cutaneous adverse food reactions
- Atopic dermatitis
- Endocrinopathies
- Hypothyroidism
- Hyperadrenocorticism
Topical therapies can be challenging and require consistent owner compliance, however there are numerous benefits3 to a consistent topical plan including:
- More rapid clearance of infections than with systemic therapies alone
- Reduced risk of future developing resistant bacterial strains on the skin in the future
- Removal of crust, organic material, allergens, and bacteria from the skin and coat
- Decreased the need for systemic antibiotics
Selecting the best topical maintenance plan is case dependent. For more information about selecting a topical plan for you patient please click here:
References
- Hillier, A., Lloyd, DH., Weese, JS., Blondeau, JM., et al. Guidelines for the diagnosis and antimicrobial therapy of canine superficial bacterial folliculitis (Antimicrobial Guidelines Working Group of the International Society for Companion Animal Infectious Diseases. Veterinary Dermatology. 2014;25: 163-e43
- Miller, WH., Campbell, KL., Griffin, CE. Mueller and Kirk’s Small Animal Dermatology 7th edition (various pages). St. Louis, Missouri: Elsevier.
- Bajwa, J. Canine superficial pyoderma and therapeutic considerations. Canadian Veterinary Journal. 2016; 57: 204-206
- Nienhoff, U., Kadlec, K., Chabern, IF., Verspohl, J., et al. Methicillin-resistant Staphylococcus pseudintermeidus among dogs admitted to a small animal hospital. Veterinary Microbiology. 2011;150: 191-197.
- Beco, L., Guaguere, E., Mendez, CL., Noli, C., et al. Suggested guidelines for using antimicrobials in bacterial skin infections (1): diagnosis based nonclinical presentation, cytology and culture. Veterinary Record. 2013; 172: 72-78.
- Beco, L., Guaguere, E., Mendez, CL., Noli, C., et al. Suggested guidelines for using antimicrobials in bacterial skin infections (2): antimicrobial choice, treatment regimens and compliance. Veterinary Record. 2013; 172: 156-160.

About the Author
Dr. Martha Lane Friedman earned her Doctorate of Veterinary Medicine from the Auburn University College of Veterinary Medicine. She completed an internship in Small Animal Medicine and Surgery at Louisiana State University, followed by a residency in Veterinary Dermatology. Dr. Friedman was board certified as a veterinary dermatologist by the American College of Veterinary Dermatology (ACVD) in 2017. She is currently providing veterinary dermatology services with Auburn Veterinary Specialists – Gulf Shores.